What is Sleep Apnea? Causes, Symptoms, and Home Remmedies
 Sleep apnea is a breathing problem or breathing disorder that occurs during sleep. To keep you safe, your brain keeps you from getting deep sleep by waking you up so you can breathe. Serious consequences can arise from this illness if left untreated. However, if patients strictly stick to their treatment plans, they usually have a relatively manageable disease.
Sleep apnea is a breathing problem or breathing disorder that occurs during sleep. To keep you safe, your brain keeps you from getting deep sleep by waking you up so you can breathe. Serious consequences can arise from this illness if left untreated. However, if patients strictly stick to their treatment plans, they usually have a relatively manageable disease.
Sleep Apnea: What is it?
Repeated pauses in breathing during sleep characterize the condition known as sleep apnea. “apnea” is derived from the Greek term for “breathless.” Sleep apnea occurs when you often wake up because you have stopped breathing. Sleep apnea can occur when your airway becomes blocked (obstructive apnea) or your brain fails to regulate your breathing (central apnea) properly.
The resultant hypoxia triggers a survival instinct, rousing you enough to start breathing again. The survival instinct wakes you up every time it kicks in. That prevents healthy sleep and has other effects, including stress on the heart, which can have serious, even fatal, repercussions.
Types of Sleep Apnea
The Three Forms of Sleep Apnea and Their Distinctive Characteristics
You already know three types of sleep apnea: obstructive, central, and complex. If you’re interested in learning more about sleep apnea treatment options and how you may get the aid you need to manage your condition, you’ve come to the right spot.
When it comes to sleep, quality is often as crucial as quantity. Even if you sleep during most of the eight-hour flight from New York to London, you probably won’t feel rested upon arrival since your body won’t have had time to progress through all of the stages of sleep necessary to do so.
What does sleepiness during an Atlantic crossing do with snoring and other sleep disorders?
The three different forms of sleep apnea all share the same underlying problem: they all prevent you from getting adequate restful sleep. When you have sleep apnea, your body cannot stay in one stage of sleep long enough to complete the tasks associated with that stage.
Sleep apnea can take many forms, each with its symptoms, but they all share one thing: they prevent you from sleeping soundly. To promote healthy sleep and help you get the amount of rest you need nightly to be aware and productive the next day, it is essential to understand the variations between each type.
What is Monkeypox? Causes, Prevention And Symptoms Of Monkeypox
In the following sections, we’ll examine these three subtypes of sleep apnea in further detail to shed light on their respective causes, symptoms, and treatment options.
OSA Refers to Obstructive Sleep Apnea.
If someone says they have sleep apnea, they may have obstructive sleep apnea, the most prevalent type. In people with (OSA), the throat and mouth muscles repeatedly relax and tense up while sleeping.
When the muscles relax, they might restrict the airway, resulting in a lack of oxygen in the lungs. This decreases the amount of oxygen in the blood, which might result in the sleeper waking up gasping for air. The cycle continues throughout the night, preventing you from getting restful sleep.
The Most Common Signs of OSA Are:

- Snoring So Loud It Can Be Heard From Another Room Drowsiness During The Day
- Some of the risk factors for OSA are within your control, while others are out of your hands.
- However, the following conditions are associated with an increased risk of OSA development.
- Although having any of these risk factors does not guarantee that you will have or develop a sleep problem, you may want to be checked out if you experience any of the following symptoms,
- particularly if your snoring worsens or your breathing pauses repeatedly while you sleep:
- Obesity
- Caused by Enlarged Tonsils and Adenoid Gland
Causes of Autism, What is Autism, Diagnosis, Treatment and Prevention
Multiple Subtypes of OSA Exist.
- Mild, moderate, and severe levels of OSA severity have been established. Each category represents the average number of times per hour when breathing is disrupted while asleep. The apnea-hypopnea index, often known as the AHI, is used to evaluate how severe sleep apnea is, including each episode as a separate occurrence.
- An AHI of 5 to 15 indicates mild sleep apnea, while an AHI of 16 to 30 indicates significant sleep apnea.
- A score of 30 or above on the AHI diagnostic scale indicates severe OSA.
- Of the almost 22 million Americans who suffer from sleep apnea, it is believed that 80% of cases fall into the moderate to severe category.
- Tracking your AHI is one way to tell if your treatment for sleep apnea is working. If your AHI is low, you get a good night’s sleep every night. The AHI readings on your CPAP machine should be less than five and might be as low as one if your therapy for sleep apnea is successful. While everyone is different, monitoring your AHI can show you how well your treatment works.
How to Deal with Sleep Disordered Breathing

In many patients, CPAP therapy is the predominant treatment modality for managing (OSA).
The CPAP machine works by continuously pumping air into the mask. Maintaining an average degree of respiratory function and an open airway during sleep is easy with constant pressure.
Using CPAP daily can help you breathe easier, get more restful sleep, and boost your health.
When lying down, anyone can develop OSA at any time of day or night. OSA can happen any time the airway muscles in the throat are relaxed enough to allow the airway to close off.
Surgery may be considered when other therapies have failed, and the cause of OSA cannot be changed (as in the case of those with a narrow throat or enormous tonsils or adenoids). (UPPP), (MMA) and (RFA) are all surgical options for treating sleep apnea.
Have You Considered Having Sleep Apnea?
If your significant other always complains about your snoring, you may have sleep apnea.
What is Lung Cancer? Symptoms, Factors, Diagnosis, Treatment, and Prevention That All You Need to Know.
Sleep Apnea, Central
Compared to OSA, CSA is a much rarer sleep disorder. In most cases, this is due to underlying brain-related health issues. In CSA, the brain cannot send the impulses for breathing. Hence, the patient does not take a breath.
Those with CSA experience respiratory distress because the brain fails to effectively signal the muscles that control breathing function, setting the condition apart from obstructive sleep apnea (OSA).
The lack of an obstruction in the airway is what sets this apart from obstructive sleep apnea. CSA can occur in people with Parkinson’s disease, who regularly use opioids, or have had a brain infection.
Some of the signs of CSA are:
- Nighttime Breathing Cessation
- Breathlessness Resolved by Sitting Up
- Nighttime Chest Pain Difficulties Focusing on Emotional States
Although the ‘lost connection’ of brain signals described here may seem like what happens during a seizure, there is no proven medical connection between epilepsy and CSA. However, sleep apnea and epilepsy have been linked.
- Many of these symptoms are similar to but distinct from, those of OSA.
- The main distinction is that a person with CSA has trouble breathing because their brain cannot convey the proper cues to their body.
- It should come as no surprise, then, that many of the events that lead to CSA have to do with compromising brain processes rather than directly affecting or blocking muscles, like in the case of OSA.

Syndrome of Cheyne-Stokes.
Cheyne-Stokes is a disorder characterized by episodes of highly shallow breathing caused by a gradual decrease in the intensity and effort of breathing. It is typically associated with congestive heart failure or stroke. The rate at which one breathes slows down and stops.
What is Bipolar II Depression? Psychopharmacologic Treatment of Bipolar II Depression
The Complicated Nature of Sleep Apnea.
When both CSA and OSA are present in the same individual, they are said to be suffering from Complex Sleep Apnea. CompSA is another name for it. In the following paragraphs, we’ll explore this topic further.
Elevated Positions. Sometimes, you start breathing more shallowly at a higher altitude. CSA thrives in environments where the air is thinner, and there is less oxygen, making it more difficult to breathe.
The Manifestations of Sleep Apnea
Sleep apnea is distinguished by abnormal breathing patterns that occur during the sleep period., which can lead to various symptoms. These symptoms encompass the nocturnal manifestations of disrupted breathing and the diurnal consequences of compromised sleep quality.
The manifestations of Obstructive Sleep Apnea
- Common manifestations of obstructive sleep apnea encompass:
- Excessive daily sleepiness (EDS) is characterized by an abnormal and persistent tendency to feel excessively sleepy throughout the daytime.
- Loud snoring is frequently accompanied by intermittent gasping or choking sounds.
- Morning headaches that may endure for several hours following awakening.
- The occurrence of xerostomia upon awakening
- The individual experiences disrupted sleep, characterized by intermittent spells of awake throughout the night.
- There is an elevated requirement to arise from a supine position to void urine.
- The individual’s emotional state is characterized by a heightened irritability or annoyance.
- The diminished level of concentration
Some symptoms associated with obstructive sleep apnea may not be readily apparent at the outset.
Initially published in 1899 as a compact reference guide intended for medical practitioners and chemists, the Manual saw further expansions in content and coverage, ultimately establishing itself as a highly regarded and extensively utilized medical compendium among professionals and the general public.
To the individual afflicted with the disease above. For instance, detecting irregular breathing and snoring may be contingent upon observing a bedmate.
The manifestation of many symptoms associated with obstructive sleep apnea may arise from other underlying health conditions, hence rendering symptomatology alone insufficient for diagnostic purposes.
According to the Scientists and Researchers, Which Fat is The Best for Brain Health?
The Manifestation of Central Sleep Apnea
The symptoms commonly associated with central sleep apnea are as follows:
- The phenomenon of atypical respiratory patterns
- Respiratory patterns, including deceleration, acceleration, and intermittent cessation, are observed during sleep.
- Excessive daily sleepiness (EDS) is characterized by an abnormal and persistent tendency to feel excessively sleepy throughout the daytime.
- Episodes of waking up during the night
- Episodes of nocturnal dyspnea or angina pectoris
- One of the challenges individuals may encounter is the ability to concentrate their attention effectively.
- The occurrence of headaches in the morning
- Like obstructive sleep apnea, individuals with central sleep apnea typically lack awareness of their abnormal breathing patterns during sleep unless they are alerted by a bed partner or carer.
Sleep apnea is a widely seen sleep disease distinguished by recurrent respiratory cessation during sleep.
The Root Causes of Sleep Apnea.


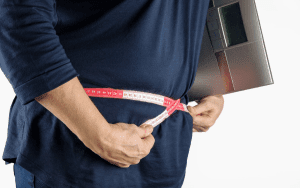
Obesity is strongly associated with the soft tissues in the mouth and throat, which makes it the primary factor contributing to obstructive sleep apnea in adults. During sleep, the relaxation of the throat and tongue muscles can obstruct airflow by the soft tissue.
More than 50% of persons diagnosed with obstructive sleep apnea have a body mass index (BMI) that falls between the overweight range (25-29.9) or the obese content (30.0+).
After the age of 60, the risk of obstructive sleep apnea (OSA) caused by a 10% increase in weight decreases.
Measuring an individual’s neck circumference can serve as an extra indicator of their body weight.
In males, a neck circumference above 17 inches (43 centimetres) and in females, a neck circumference beyond 15 inches (38 centimetres) is associated with a notable elevation in the likelihood of developing obstructive sleep apnea (OSA).
What is Aphasia? A Communication Issue
Additionally, OSA can also be caused by or made worse by the following factors:
- The airway is restricted.
- A crown with a dome shape.
- Hypothyroidism
- Acromegaly, also known as hormonal overgrowth, is a condition that affects the body’s hormone levels.
- I have allergies.
- Septal deviation refers to a structural issue that affects the nose.
- Various illnesses can lead to the accumulation of mucus in the trachea and bronchi.
- Smoking
- Drug or alcohol misuse
- Swollen tonsils or adenoids and dental problems like a significant overbite are common causes of obstructive sleep apnea in young individuals.
- Rare causes of airway obstruction include tumours or growths in the airway and congenital anomalies such as Down syndrome and Pierre-Robin syndrome.
- People with Down syndrome have less developed muscles in the upper airway and an enlargement of the tongue, adenoids, and tonsils.
- Pierre-Robin syndrome is a condition that is characterized by a small lower jaw and a language that tends to curl and rest towards the back of the throat.
- Obstructive sleep apnea is associated with both childhood and adult obesity. However, it is less common in children compared to adults.
There is an established correlation between the lack of treatment for obstructive sleep apnea and specific outcomes with cardiovascular illness, accidents, and premature death in individuals of all age groups.
Suppose someone is experiencing symptoms of obstructive sleep apnea, such as loud snoring, frequent awakenings during the night, and excessive daytime fatigue. In that case, they need to seek evaluation from a doctor.
Earlier Onset of Respiratory Infections in Children, According to the CDC.
What Actions Can I Take to Address This Issue?


Treating physicians often do not know the underlying cause of CSA. Medical professionals refer to this form of CSA as “primary” or “idiopathic.”
However, in some cases, instances of CSA can be attributed to a different condition, drug, or environmental factor.
The Cheyne-Stokes breathing pattern is abnormal breathing characterized by alternating periods of deep, rapid breathing followed by periods of shallow, slow breathing, or even CSA caused by various medical conditions such as stroke, heart attack, or kidney failure. The medical community recognizes these symptoms as CSB-CSA.
Non-CSB CSA can be caused by various medical conditions such as heart disease, kidney disease, and other factors.
High-altitude central sleep apnea (CSA) typically occurs when individuals sleep above 15,000 feet. You should start feeling better once you return to sea level.
Hydrocodone and fentanyl are commonly prescribed opiates that can potentially cause Central Sleep Apnea (CSA). It is possible that a medication adjustment prescribed by your doctor could be helpful.
It is strongly recommended that individuals who suspect they may be misusing prescription drugs, especially opiates, seek professional assistance.
The Cause of CSA in Infants is Often Unknown and Referred to as Idiopathic.
Several factors can disrupt the brain impulses that generally help your child breathe. These factors may also contribute to child sexual abuse (CSA):
- The delivery was made ahead of schedule.
- Tobacco use during pregnancy
- Malignant brain tumours
- Cerebral Palsy: Understanding the Disorder
- I have a punctured head.
- Issues that originate in the brain stem, also known as the base of the skull.
I would like to know more about the statistics related to sleep apnea.
Obstructive sleep apnea, estimated to affect 4-9% of middle-aged adults, often remains undiagnosed and untreated. It is estimated that approximately 10% of the elderly population is affected.
As individuals age, the brain’s capacity to keep the upper airway muscles, such as the throat, firm during sleep diminishes. This decline in function raises the likelihood of airway narrowing or collapse.
Sleep apnea is a condition that is more prevalent among women during pregnancy and after menopause, despite men exhibiting a higher prevalence of obstructive sleep apnea, which can be up to four times greater. After women enter menopause, the gender discrepancy among elderly adults decreases.
The use of hormone replacement therapy, specifically with progesterone and/or estrogen, has decreased the likelihood of postmenopausal women developing obstructive sleep apnea compared to those who do not use these hormones.
However, hormone replacement therapy is not considered a viable treatment option due to its potential adverse effects.
Furthermore, there is a correlation between obstructive sleep apnea and the following factors:
- Origin stories explain the beginnings or backgrounds of certain entities, such as characters, events, or concepts.
- A family history of OSA in 25%-40% of patients indicates a potential genetic susceptibility to the condition, implying a predisposition toward health problems.
- I would like to discuss the topic of ethnicity. African Americans, Hispanics, and Pacific Islanders have a higher prevalence of sleep apnea than whites.
Risk Factors Associated With Sleep Apnea
Understanding the risk factors associated with sleep apnea is crucial for identifying those more susceptible to developing this condition.
Various determinants influence an individual’s susceptibility to developing sleep apnea, including distinct factors associated with OSA) and CSA).
The present study aims to identify and analyze the risk factors linked with obstructive sleep apnea.
- The predominant risk factors associated with obstructive sleep apnea are age, gender, body mass index, and specific anatomical characteristics of the craniofacial region.
- Age is a significant factor in the likelihood of getting obstructive sleep apnea, with the risk steadily increasing until someone reaches their sixties and seventies.
- Gender: Individuals who are male or assigned male at birth tend to exhibit a higher propensity for obstructive sleep apnea, particularly during the initial phases of adulthood.
- Individuals with sleep problems because of obstructive exhibit specific anatomical characteristics, such as an enlarged tongue and a diminished mandibular length, within the context of head and neck anatomy.
- Numerous studies have shown that an individual’s risk of developing obstructive sleep apnea increases proportionally to their body mass index (BMI).
- Numerous studies have established correlations between several factors and a heightened probability of experiencing obstructive sleep apnea (OSA); nevertheless, additional study is required to elucidate the impact of these factors on the onset and progression of OSA.
- Cigarette smoking has been a factor with a significantly increased likelihood of developing obstructive sleep apnea, as indicated by several research studies, in comparison to individuals who have either ceased smoking or never engaged in smoking behavior.
- Hormonal disorders, such as hypothyroidism or hypersecretion of growth hormone, have potentially elevated susceptibility to obstructive sleep apnea (OSA).
- By inducing tissue inflammation.
- Proximity to the respiratory passage or the act of increasing one’s body mass index can both be factors that contribute to this phenomenon.
- The sleeping position could develop or exacerbate sleep apnea, especially when individuals choose a supine position.
- The impact of the sleeping posture on the morphology and location of the tissue around the airway is a contributing factor.
- Evidence suggests that individuals with a familial obstructive sleep apnea (OSA) background may be susceptible to developing this condition. This heightened risk could be attributed to common anatomical characteristics in the craniofacial region among family members.
- Nasal congestion, characterized by nasal airflow obstruction, increases obstructive sleep apnea (OSA) propensity.
- The consumption of alcohol and certain medications is correlated with an increased likelihood of experiencing obstructive sleep apnea.
- Certain medical illnesses can increase the susceptibility of individuals to develop obstructive sleep apnea (OSA). This includes those with various heart and lung issues.
The present study aims to investigate the many risk variables connected with central sleep apnea (CSA). Central sleep apnea (CSA) is a sleep disease distinguished by the periodic halt or reduction of breathing effort during sleep. This occurs due to the brain’s inability to deliver proper signals to the respiratory muscles. It is vital to comprehend the risk factors associated with child sexual abuse (CSA).
An underlying medical problem, like a brain stem infection or injury, is often detected in those with central sleep apnea.
The Process of Diagnosing Sleep Apnea
The diagnosis of sleep apnea necessitates the involvement of a medical professional or sleep specialist. It encompasses a series of sequential phases in the diagnostic procedure.
The initial step in assessing sleep apnea generally involves a comprehensive examination of an individual’s symptoms and overall well-being and a thorough physical examination. The purpose of this system is to discover indicators of sleep apnea and ascertain potential risk factors that may contribute to the development of this illness.
While it is necessary to conduct tests to establish a definitive diagnosis of OSA, the manifestation of symptoms can play a role in the diagnostic process and aid in assessing the extent of the problem.
To ascertain the presence of obstructive or central sleep apnea, it is imperative to conduct a sleep study. Polysomnography, the most reliable form of sleep research, is often administered within a dedicated sleep laboratory setting, requiring an overnight stay.
Polysomnography involves the utilization of various sensors to monitor respiratory patterns, arousals, oxygen saturation, muscular activity, sleep phases, and additional sleep-related parameters.
An in-clinic polysomnography can assess the presence of abnormal breathing patterns during sleep and distinguish between obstructive sleep apnea and central sleep apnea. Polysomnography for obstructive sleep apnea (OSA) may encompass a single or dual attendance at a sleep clinic facility.
An alternative is an at-home sleep study for patients suspected of more severe obstructive sleep apnea (OSA). Although conducting a sleep apnea test at home may offer greater convenience, it is imperative to note that the interpretation of the data still necessitates the involvement of a qualified healthcare practitioner. Central sleep apnea is not typically diagnosed using home testing methods.
The Process of Diagnosing Sleep Apnea
Confirming sleep apnea as a diagnosis necessitates conducting a sleep study to verify the presence of respiratory disturbances during sleep. To ascertain the necessity of a referral for a sleep study, a physician will initially do a comprehensive physical examination, inquire about presenting symptoms, and gather pertinent personal and familial medical background.
During the process of assessing sleep apnea, a medical practitioner may inquire about one or many aspects by posing the following queries:
Do you have feelings of fatigue or drowsiness during the day?
Have you received any reports of snoring or episodes of breathing cessation during your sleep?
Is maintaining wakefulness while driving, reading, or watching television challenging?
Have you ever engaged in smoking behavior, either presently or in previous periods?
Has any member of your family received a diagnosis of sleep apnea?
- During the examination, the physician may investigate factors such as weight, neck circumference, blood pressure, and other medical disorders contributing to increased susceptibility to sleep apnea. Certain medical professionals may require individuals to complete a survey regarding their sleep patterns.
- If the physician harbors suspicions about sleep apnea following a comprehensive examination and evaluation of symptoms, they will probably advise the patient to do a sleep study.
- A polysomnogram is a diagnostic test used in sleep medicine to monitor and record various.
- A polysomnogram is a sleep study wherein medical sensors are employed to observe and record an individual’s respiratory patterns, cardiac rhythm, and electroencephalographic (EEG) brain wave activity during sleep.
- To receive a diagnosis of sleep apnea, an individual must undergo a polysomnogram, which can be conducted either in a sleep laboratory or within the confines of their own home.
- When undergoing a polysomnogram at a sleep laboratory, individuals will receive specific instructions from their healthcare practitioner regarding the recommended arrival time, necessary items to carry, and any dietary or medication adjustments that may be required on the day of the procedure.
- Upon familiarising oneself with the assigned sleeping quarters inside a laboratory setting, a technician affixes monitoring sensors onto several anatomical regions, including the legs, fingers, chest, and head.
- During sleep, the sensors measure various physiological processes occurring within the body. The collected data is subsequently transformed into distinct categories representing different stages of sleep, wakefulness, and instances characterized by interrupted breathing.
- Suppose a physician deems it probable that an individual is afflicted with sleep apnea. In that case, they may prescribe a sleep study, including a trial of a positive air pressure (PAP) device. This type of sleep study is sometimes called a split-night sleep study.
- If the polysomnogram findings obtained during the initial portion of the night validate the presence of substantial sleep apnea, a positive airway pressure (PAP) device will be administered and tailored throughout the latter part of the night to facilitate the initiation of continuous treatment.
- The utilization of a positive airway pressure (PAP) device serves the purpose of maintaining the patency of the soft tissues inside the respiratory tract. This is achieved by directing the air that is pressurized and humidified through a conduit and a facial mask, both affixed during sleep.
- The PAP device is utilized to assess the impact of varying air pressures on an individual’s physiological activities to determine the optimal pressure setting.
- A polysomnogram conducted in a sleep center may be more advantageous than a home sleep apnea test under certain circumstances. These circumstances include heart or lung disease, risk factors associated with central sleep apnea, or the likelihood of being diagnosed with other sleep disorders.
- The utilization of a home sleep apnea test (HSAT) is a viable alternative for individuals who exhibit symptoms, possess a medical history, and undergo signs of moderate to severe sleep apnea on physical examination.
- Physical examination that suggests the presence of mild to severe obstructive sleep apnea. The HSAT (Home Sleep Apnea Test) requires a smaller number of measures compared to an in-lab sleep study and lacks the inclusion of brain sensors (EEG) and muscle sensors (EMG) that are utilized to evaluate sleep or sleep stages.
- However, it should be noted that home sleep apnea testing does offer certain advantages. For instance, those who sleep within the familiar confines of their residence tend to have extended durations of sleep. Using an HSAT can also assess the efficacy of a PAP device or reassess an individual who continues to exhibit symptoms despite commencing treatment.

Various home sleep apnea test kits are already available, and your sleep specialist is responsible for providing guidance on the appropriate utilization of the sensors.
After an examination, the medical practitioner carefully examines the gathered data and collaborates with the patient to determine the most optimal treatment plan.
Diagnostic Criteria
- The diagnostic criteria refer to a set of standardized guidelines used in clinical practice to assess and identify the presence of a particular disorder or condition.
- The determination of obstructive sleep apnea is reliant upon the findings of the polysomnogram and the identification of specific symptoms.
- Apnea refers to the cessation of airflow for 10 seconds or more.
- Hypopnea is a respiratory condition characterized by shallow breathing lasting at least 10 seconds, resulting in a decrease in blood oxygen levels or a momentary sleep disruption.
- Respiratory effort-related arousal (RERA) refers to instances in which breathing is mildly restricted, not as severely as in a hypopnea, yet nonetheless leads to a momentary waking from sleep.
- Typical manifestations of sleep apnea are excessive daytime somnolence, nocturnal snoring, and matutinal cephalalgia. Infrequently, individuals may encounter episodes of insomnia or nocturnal awakenings accompanied by a need to urinate.
- The diagnosis of sleep apnea is established when a minimum of five respiratory episodes per hour of sleep are documented during the sleep study.
- The assessment of sleep apnea severity is predominantly based on the average frequency of respiratory attacks occurring per hour. In conjunction with symptoms and medical background, this metric is a basis for determining appropriate treatment modalities.
- Accurately identifying central sleep apnea necessitates thoroughly evaluating an individual’s symptoms and polysomnography results. Nevertheless, central sleep apnea has various subtypes, each characterized by distinct diagnostic criteria.
Treatment: Therapeutic Interventions for Sleep Apnea

Several available non-invasive therapy modalities for sleep apnea have varying degrees of efficacy. Non-surgical alternatives can be classified into positive airway pressure (PAP) devices and oral appliances.
(CPAP) is a Medical Intervention Commonly Used in the Treatment of Sleep Apnea.
(CPAP) is widely regarded by health experts as the preferred treatment modality for obstructive sleep apnea (OSA). Typically, it is the initial therapeutic intervention recommended to individuals diagnosed with moderate to severe OSA.
Typically, (CPAP) equipment is connected to a power source and positioned near the bed of the individual using it. A cylindrical conduit establishes a connection between the apparatus and a facial covering that encompasses the individual’s oral and/or nasal regions in sleep.
Subsequently, the continuous positive airway pressure (CPAP) machine delivers air into the individual’s respiratory passage, assisting in maintaining its patency during the sleep cycle.
Continuous positive airway pressure (CPAP) is often regarded as the most efficacious treatment for obstructive sleep apnea (OSA); nonetheless, its effectiveness is contingent upon consistent nightly usage. CPAP therapy’s efficacy in treating central sleep apnea is comparatively lower.
(CPAP) machines are designed to deliver a consistent airflow rate, which the physician determines based on the average requirement of the individual sleeper. Given that specific individuals may experience difficulties sustaining sustained air pressure levels, alternative options are accessible.
Bilevel Positive Airway Pressure (BiPAP)
Bilevel Positive Airway Pressure (BiPAP) is a therapeutic intervention commonly used in the medical field to manage respiratory conditions.
In some instances, medical practitioners may administer a bilevel positive airway pressure (BiPAP or BPAP) machine as an alternative to pressure (CPAP) for individuals experiencing difficulties tolerating the latter due to sleep apnea.
The BiPAP machine functions analogous to the CPAP machine, wherein an interconnected tube delivers pressurized air to a mask to maintain airway patency. Nevertheless, a distinction exists between a BiPAP machine and a CPAP machine regarding the air pressure it provides.
Specifically, a BiPAP machine administers air at elevated stress during the inhalation phase of sleep. At the same time, during exhalation, it has an atmosphere at a reduced pressure.
The characteristic above renders BiPAP therapy a favorable option for individuals experiencing difficulty exhaling against the elevated air pressure delivered by a CPAP machine. BiPAP machines are occasionally recommended for individuals with sleep apnea, severe obesity, and specific medical disorders such as chronic obstructive pulmonary disease and hypoventilation.
Auto-Adjusting Positive Airway Pressure (APAP)


Is a therapeutic modality to treat sleep-related breathing disorders, such as obstructive sleep apnea. APAP devices are designed to automatically adjust the level of positive airway pressure
Auto-adjusting positive airway pressure (APAP) devices, commonly referred to as APAP or auto-CPAP machines, function in a manner comparable to continuous positive airway pressure (CPAP) machines. APAP machines are distinguished from CPAP devices by their capacity to autonomously regulate the air pressure they deliver.
The capability above has the potential to enhance the user experience of the machine in comparison to a CPAP device. Individuals may require varying pressure levels during the night based on their sleeping position or other relevant considerations.
APAP machines employ pressure sensors and a computer algorithm to automatically titrate, i.e., determine the precise air pressure required by an individual throughout various stages of sleep.
Consequently, those who experience discomfort due to the continuous air pressure emitted by a CPAP machine may find that an APAP machine offers improved efficacy. Sleep experts can configure APAP machines to only deliver air at pressures within a predetermined range, thus enhancing its effectiveness.
Adaptive Servo-Ventilation (ASV)
Is a therapeutic approach to manage sleep-disordered breathing.
Adaptive servo-ventilation (ASV) is generally employed as a therapeutic intervention for those afflicted with central sleep apnea. The operation of ASV is comparable to that of PAP therapy, as it involves the delivery of pressurized air through a tube and mask worn by the individual during sleep.
In contrast to providing a fixed air volume during inhalation and exhalation, Adaptive Servo-Ventilation (ASV) is designed to give personalized air pressure that dynamically adjusts in response to central apneic events, anticipating and addressing them in real time.
Initially, Adaptive servo-ventilation (ASV) was employed as a therapeutic intervention for Cheyne-Stokes respiration. This distinct respiratory pattern may manifest as a consequence of heart failure.
The user’s text needs to be longer to be rewritten academically. Adaptive servo-ventilation (ASV) has effectively managed central sleep apnea (CSA) within specific parameters. However, research findings indicate that ASV may provide significant risks for those presenting with both CSA and some forms of severe congestive heart failure.
Expiratory Positive Airway Pressure (EPAP)
A therapeutic technique for treating respiratory disorders, particularly obstructive sleep apnea.
In contrast to the motorized CPAP and BiPAP sleep apnea treatments, the expiratory positive airway pressure (EPAP) equipment does not possess motorized functionality.
The EPAP therapy comprises a pair of tiny valves that are inserted into the nostrils. EPAP therapy generates resistance to maintain airway expansion during exhalation, delivering airway pressure.
EPAP therapy may offer enhanced convenience for specific individuals due to its low reliance on energy, little noise production, and compact and lightweight design. The efficacy of nasal expiratory positive airway pressure (EPAP) therapy has primarily been assessed in individuals diagnosed with obstructive sleep apnea (OSA) rather than those with central sleep apnea (CSA).
EPAP therapy is a relatively recent development in positive airway pressure (PAP) therapies, and its prescription rate is comparatively lower compared to other PAP therapies. Nevertheless, a comprehensive analysis of studies on Expiratory Positive Airway Pressure (EPAP) revealed that individuals utilizing EPAP techniques observe a decrease of 53% in their symptoms.
Sleep Apnea’s Toll on Your Respiratory System
Asthma and COPD can be made worse by sleep apnea because of the lack of oxygen in the body when sleeping. You may have increased fatigue and shortness of breath during physical activity.
Hormonal and Endocrine

Cells that don’t respond appropriately to the hormone insulin are known as insulin resistance, and it’s more common in those who suffer from sleep apnea. Lack of proper insulin uptake by cells is a significant facter to the development of type 2 diabetes.
Sleep apnea has also been associated to the metabolic syndrome, which includes hypertension, high LDL cholesterol, high blood sugar, and a larger-than-average waist circumference.
Organs of Digestion
Fatty liver disease, scarring, and elevated liver enzyme levels are more common in those with sleep apnea.
Apnea can make Heartburn and other symptoms of gastroesophageal reflux disease (GERD) worse by apnea, further disrupting sleep.
The Cardiovascular and Circulatory Systems
Obesity and hypertension, exacerbated by sleep apnea, stress the cardiovascular system more. An irregular heart rhythm like atrial fibrillation, more common in those with apnea, can raise the risk of stroke. Sleep apnea is deep with an increased risk of heart failure.
Brain and Nerves
Central sleep apnea occurs when the brain’s impulses that control breathing become disrupted. Numbness and tingling are other neurological symptoms associated with this form of sleep apnea.
Physiology of Reproduction
Having sleep apnea can make you less sexually motivated. Erectile dysfunction and a man’s fertility could be negatively impacted.
Diverse Structures
- Sleep apnea symptoms often include, among others:
- dry
- morning soreness in the mouth or throat
- headache
- trouble taking notice
- irritability
What is the Severity of Sleep Apnea, and When Should I be Concerned?


The impact of sleep apnea varies among individuals. On average, adults take a break five times per hour, whereas children take a break once per hour. These occurrences are assumed to happen naturally during REM sleep.
A sleep study can be used to detect Obstructive Sleep Apnea (OSA) when a patient who frequently experiences breathing problems during sleep requests it. Sleep apnea is categorized into the following subtypes:
- Mild: A frequency of 5-14 occurrences per hour is considered mild.
- Moderate symptoms typically range from 15 to 30 times per hour.
- Extreme weather conditions are 30 or more events within one hour.
Tracking oxygen deprivation is another crucial factor to monitor during these times. Hypoxemia is a medical condition where the oxygen level in the blood is 90% or lower.
In the presence of heart or lung illness, each apnea episode can lead to a notable decrease in oxygen levels. As a result, the body may experience heightened stress levels during the night. There have been theories about oxygen deprivation’s potential short-term and long-term effects.
Is Sleep Apnea a Potentially Life-Threatening Condition?
It is doubtful that pauses in breathing caused by sleep apnea would result in immediate death, as the cessation of breathing is not the sole outcome. However, OSA increases the likelihood of developing severe health issues, some of which may lead to unforeseen fatalities.
The potential dangers that may result from specific actions or situations.
- The sudden cessation of breathing significantly increases the likelihood of experiencing cardiac arrhythmia, atrial fibrillation, heart attack, and stroke.
- These incidents occur more frequently in the morning, coinciding with the higher prevalence of REM sleep and sleep apnea. According to studies, individuals with OSA are 2.5 times more likely to experience sleep-related deaths between midnight and 6 a.m.
A CPAP machine, combined with other options such as dental appliances, decreases the risk of significant issues, including long-term heart problems.
Ongoing Hazards
- Untreated sleep-disordered breathing has been associated with significant health issues when it persists over a prolonged period. The prevalence of high blood pressure, diabetes, and cardiovascular disease may increase.
- It can lead to feelings of sadness, memory impairment, daytime drowsiness, and potentially even accidents.
- While obstructive sleep apnea (OSA) itself may not be lethal, it can lead to various complications that can be life-threatening. This emphasizes the importance of addressing sleep apnea for your overall health.
Home Remmedies
Here are some ideas to improve your sleep and decrease apnea.The (CPAP) mask is widely used to treat sleep apnea.
While it does the job, some may feel uneasy using it. The same effects could be achieved with several home treatments. The following are six non-traditional methods for treating sleep apnea.
1, Try to Keep a Healthy Weight.
Those who suffer from sleep apnea are often advised to reduce their body mass index. Upper-body obesity is associated with a higher prevalence of airway blockage and constricted nasal passageways. These blockages can result in brief or prolonged episodes of apnea during sleep.
Sleep apnea symptoms can be mitigated by sticking to a healthy weight.If obese patients lose even a small amount of weight, they reduce their risk of needing upper airway surgery and prolonged CPAP therapy.
Losing excess weight can sometimes cure sleep apnea. However, the problem may return if the weight is regained.
Do Some Yoga.
Studies have indicated that maintaining a regular exercise routine can improve energy levels, cardiac health, and sleep quality. In particular, practicing yoga can improve your lungs and increase oxygen intake.
Reduced blood oxygen saturation is linked to sleep apnea. The breathing exercises in yoga have been shown to increase blood oxygen levels. Therefore, yoga lessens the number of times you have to get up during the night.
3, Try a New Sleeping Posture.
Even though it’s a simple adjustment, switching your sleeping posture can alleviate sleep apnea and help you get a better night’s rest. Over 50% of obstructive sleep apnea cases rely on posture, according to a study conducted in 2006.
Sleeping in the supine position, often known as on one’s back,
Children with sleep apnea tend to sleep better on their backs, according to a 2002 research
Talk to yourmedical supervisor about your sleep apnea symptoms and how your body placement could contribute to them.
4, You Should Get a Humidifier.
A humidifier confidently adds moisture to the air. The skin and respiratory system are both more likely to react negatively to dry air. By dissolving mucus and relaxing muscles in the air passages, a humidifier helps improve breathing.
The efficiency of a humidifier can be enhanced by adding essential oils to it, such as those of lavender, peppermint, or eucalyptus. The anti-inflammatory and calming effects of these three essential oils are well-documented.
When cleaning your humidifier, make sure to do it as directed. Molds and bacteria can grow in their crevices.
-
Don’t Indulge in Tobacco and Booze
Changing your way of life can positively affect your health, including better sleep. To lessen the severity of sleep apnea, consider reducing tobacco use and alcohol consumption.
Alcohol slows your breathing because it relaxes the muscles in your throat. This can cause sleep disruptions and snoring. It can also cause inflammation in the airways, which can make it difficult to breathe.
Like alcohol, tobacco use can aggravate already sensitive airway tissue. Snoring and sleep apnea could become worse as a result of this.
Smoking was found to increase the likelihood of having sleep apnea in a study conducted in 2012. The study found that treating sleep apnea could aid in smoking cessation since patients with sleep apnea may be predisposed to smoking.
6, Make Use of Dental Aids.
The jaw or tongue can be repositioned with an oral appliance to prevent obstructive sleep apnea.
Mandibular advancement devices and tongue stabilization devices are the two primary types. These devices assist in the repositioning of the tongue or lower jaw, so creating additional room in the posterior region of the throat.
It is recommended by dentests the use of oral appliances as a therapeutic intervention for sleep apnea.
Oral appliances are recommended for persons with sleep apnea who cannot use a CPAP machine, according to guidelines published in 2015. This recommendation favors custom-fit devices over over-the-counter remedies because of the increased control over jaw alignment that they provide.
For more interesting stories click here,