What is Monkeypox? Causes, And Symptoms Of Monkeypox
 The symptoms of monkeypox exhibit more subtlety, rendering them more challenging to detect and monitor. Additionally, these symptoms may resemble those associated with the context of sexually transmitted infections; examples include syphilis and herpes.
The symptoms of monkeypox exhibit more subtlety, rendering them more challenging to detect and monitor. Additionally, these symptoms may resemble those associated with the context of sexually transmitted infections; examples include syphilis and herpes.
What is Monkeypox?
The monkeypox virus is an orthopoxvirus that results in pox (monkeypox), a condition with symptoms comparable to smallpox but less severe. Even though smallpox was eliminated in 1980, mpox still exists in some central and western African nations.
Outside of Africa, instances have been reported since May 2022 from nations with no history of pox transmission. The monkeypox virus has been divided into two separate clades: Clade I, formerly known as the Congo Basin (central African) clade, and Clade II, formerly known as the West African clade.
Mpox is a zoonosis, a disease spread from animals to humans, and cases are frequently seen near tropical rainforests where the virus-carrying animals can be found.
Squirrels, Gambian pouched rats, dormice, and many kinds of monkeys, among other animals, have shown signs of monkeypox virus infection.
Humans can also contract the sickness from other humans. Disease transmission can occur through direct or indirect contact with infected fluids, wounds on the skin or internal mucosal surfaces (such as the mouth or throat), respiratory droplets, or infected items.
The preferred laboratory test for mpox is polymerase chain reaction (PCR) viral DNA detection. The best diagnostic samples come straight from the rash and include skin, fluid, crusts, or, in some cases, a biopsy.
Methods for detecting antigens and antibodies that do not differentiate amongst orthopoxviruses may not be helpful.
What is Narcism? What is Narcism Personality Disorder in Men?
Background
Acquired immunodeficiency syndrome (AIDS) is brought on by the human immunodeficiency virus (HIV), and additional viruses, including Dengue, Zika, Ebola, and West Nile, have emerged recently, causing several new pandemics.
2, was recently identified. Causing the pandemic of the coronavirus disease 2019 (COVID-19). Several diseases can cause acute neurologic sequelae, such as long-term COVID-19, to manifest.
While COVID-19 continues killing hundreds of people yearly, MPXV has only recently emerged as a potential pandemic replacement.
The aftereffects of these VIRAL OUTBREAKS, particularly the enduring symptoms of these illnesses and their associated psychological ramifications, drive long-term public health and socioeconomic costs.
The Findings of the Current Research;
Given the lack of information on the long-term consequences of various viral infections, the current study emphasizes the post-acute neurological issues that arise after infection with smallpox and MPXV.
A zoonotic virus in the genus Orthopoxvirus is the source of both smallpox and MPXV. As a result, both viruses may cause neurological problems after infection, though to differing degrees of severity and regularity.
Viral Traditional
There are 17 orthopoxviruses, all zoonotic viruses that can infect people and animals. Human illnesses are frequently spread by feces, skin lesions, and respiratory droplets.
While other orthodox viruses do not cause disease in people, MPXV is the main cause of human illness. Rodents are the MPXV’s natural reservoirs, making the virus’s eradication a difficult task.
In May 2022, an MPXV outbreak spread to regions of Europe, North America, and Australia that are not endemic. The West African (W.A.) lineage of MPXV, now known as lineage II, appeared to be the virus most frequently observed in the general population throughout this outbreak.
Due to its prevalence among MSM, sexual transmission has been hypothesized as the main method of MPXV transmission. On September 25, 2022, roughly 65,000 MPXV cases were reported worldwide.
Causes of Autism, What is Autism, Diagnosis, Treatment and Prevention
What Does the Expert Think;
However, infectious disease specialist Dr. Jason Zucker from Columbia University in New York City, who has treated patients with monkeypox, says that the disease may be “harrowing” and has been “creating a lot of misery,” particularly among young and middle-aged men who have sex with men.
The pain originates from the sickness-induced, fluid-packed learning. Zucker notes that while some individuals have been admitted to the hospital with potentially deadly complications, including breathing difficulties or brain swelling, pain treatment is the most common cause for admission.
When Compared to the past;
Overall, doctors have seen fewerPlesions in this outbreak compared to earlier ones in Africa. On the other hand, mucosal lesions are on the rise. Lesions on the hands, feet, and faces were the most common sites for early manifestations of this condition.
As Zucker says, it’s not always the case that mucosal lesions are the worst. However, because they irritate sensitive tissue, they can cause unbearable agony, making swallowing, eating, drinking, urinating, and defecating difficult or impossible.
These lesions are much more difficult to identify and characterize than skin cancer. McCollum suggests that the number of lesions counted as a surrogate for the degree of illness on the World Health Organization’s (WHO) severity scale for monkeypox may need to be adjusted.
Significant Repercussions
Deaths from the worldwide outbreak of monkeypox have been documented in at least eleven countries. The extent to which the virus was responsible for these deaths is currently being studied.
The two victims, Americans and Mexicans, had compromised immune systems and died of unrelated causes. (These deaths are being investigated by the CDC as possible monkeypox cases.
Two people in Spain with no additional risk factors died from encephalitis, sometimes known as brain swelling. McCollum agrees that the mortality toll is “definitely disturbing, but not wholly shocking,” citing the historical prevalence of monkeypox.
According to Zucker, encephalitis is a rare but fatal complication of numerous other types of viral infections; the origin of brain swelling in monkeypox encephalitis is unknown at this time but may be due to either the virus penetrating brain tissue or an overactive immune response.
A review of the literature published on September 8 found evidence that patients with monkeypox have experienced seizures and encephalitis in the past. Only 3.0 percent of the 1,512 people surveyed fell into this category.
Jonathan Rogers, a neuropsychiatrist at University College London and a co-author of the study, explains, “We have to move beyond merely thinking monkeypox a skin and respiratory illness.“
Even though the monkeypox virus has evolved since earlier outbreaks, the virus’s wider and more varied current host population has provided researchers with new information.
What is Lung Cancer? Symptoms, Factors, Diagnosis, Treatment, and Prevention That All You Need to Know.
Exactly Where Did this Pandemic Start?
The animation features a man sick with viruses with rodents, equines, and camels.
The virus behind this pandemic has striking similarities to those found in Nigeria. There were no reported cases of monkeypox in the country between the years of 1979 and 2016. Even yet, in September 2017, an 11-year-old child became sick and started an epidemic.
Increased surveillance the next year led to identifying 276 suspected or confirmed cases. Warnings from the government suggest that monkeypox may have been circulating widely in the country for some time.
Human-to-human transmission replaces animal-to-human transmission in the Nigerian outbreak, at least in urban areas and correctional facilities.
The Number of People Infected With the Virus Continued to Rise.
Approximately 66,000 cases have been confirmed since spring 2022, with the United States accounting for over a third. (WHO) announced the outbreak as a global health emergency on July 23, signaling that this outbreak is severe and calling for international collaboration.
Since monkeypox is not a new disease, we know much about it. We’re looking into it even more to find out things like whether or not this event is permanent.
Suffering From the Smallpox Virus
In 1980, the World Health Organisation (WHO) formally declared the smallpox virus extinct after decades of epidemics on numerous continents. Variola major and minor are the two kinds of smallpox virus, with primary variola infection frequently being more severe and having a greater fatality rate.
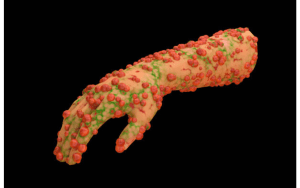
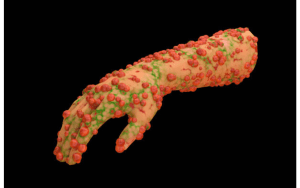
Symptoms of Monkeypox
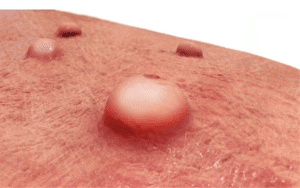
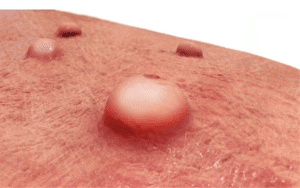
In the symptoms of monkeypox, People frequently get a rash that might appear on their hands, feet, chest, face, or mouth and close to their genitalia, such as the penis, testicles, labia, vagina, and anus. Incubation lasts from three to seventeen days. During this time, a person’s symptoms may be nonexistent or feel completely normal.
There will be multiple stages, including scabbing before the rash heals.
The rash may appear as bumps or blisters initially and cause some discomfort.
Additional signs and Symptoms of Monkeypox include
- Fever
- Chills
- enlarged lymph nodes
- Exhaustion
- Back pain and muscle aches
- Headache
- respiratory signs (such as a cough, sore throat, or nasal congestion)
You can encounter all of the symptoms or just a few.
After your previous exposure, you have 21 days to look for mpox signs. Visit a doctor if you get symptoms like a rash.
Rashes on the skin (usually with elevated blisters) and high body temperatures are two telltale signs. Generally, when someone says their disease is “mild,” they mean it hasn’t progressed to the point where they need medical attention in a hospital, or it hasn’t killed them.
Many people who have had blisters have said the pain was unbearable.
What do we know about the virus itself, if anything?
DNA is used as the genetic material in orthopoxviruses (as opposed to RNA in SARS-CoV-2 or influenza viruses). DNA viruses also develop more slowly than RNA viruses. The term “pox” originally referred to the blisters brought on by such viruses.
Among these are the viruses that cause diseases in various animals, such as camelpox, horsepox, cowpox, and raccoon pox.
(Chickenpox is glaringly absent from this list. Despite sounding like the pox virus and displaying some of the same symptoms, this is a type of herpes. Since they are zoonotic, most common viruses can easily jump from animals to people.
The smallpox virus probably first appeared in rodents. Natural selection facilitated its adaptation to human hosts, facilitating its spread from one human to another.
How Long do the Symptoms of Monkeypox Last?
The first signs of measles normally appear three weeks after introducing the virus. When experiencing flu-like symptoms, a rash typically appears 1-4 days later.
From the time symptoms appear until the rash has totally recovered and a new layer of skin has developed, a person with pox can transmit it to others.
According to recent Research, some persons can transmit the pox to others one to four days before symptoms manifest. It’s unclear how many people the current outbreak has impacted.
There is no proof that those who never experience symptoms have transferred the virus to another person. The most recent data about the spread of pox will continue to be monitored by the CDC.
The central nervous system’s impact on the smallpox and monkeypox viruses
Brain Damage Caused by MPXV
Neurological effects of smallpox might include headaches, backaches, encephalopathy, psychosis, and seizures at different phases of the illness.
Encephalitis can occasionally result from cerebral fluid cultures that lack neutrophil evidence (CSF). When the nervous system is affected, a slight increase in protein levels and a normal range of glucose levels are also observed.
People with the older smallpox vaccination had a 25% higher chance of dying from sequelae, such as postvaccinal encephalomyelitis (PVEM). Older smallpox vaccines are no longer utilized since more recent vaccines have higher biosafety profiles.
Neurological recovery from an MPXV infection is not always followed by a complete resolution of all symptoms. Skin lesions developed to the point of opening can cause dysphagia, anal fissures, and rectal pain. A central nervous system (CNS) infection can worsen by conjunctivitis, leading to temporary blindness.
Urgent Medical Attention is Required;
If you think you might have an STD. Regional health departments should do PCR and serology tests on the vesicular fluid in all cases. Cerebrospinal fluid (CSF) analysis may be required if neurological symptoms are present.
When symptoms appear suddenly, especially in the brain, it’s important to do biological testing to identify the causative culprit. It is recommended to check the CSF for MPXV DNA and conventional viral immunoglobulin (Ig)M.
Possible Monkeypox-Related Complications
Mpox can cause a variety of problems.
- bronchopneumonia
- sepsis
- Encephalitis, or inflammation of brain tissue.
- corneal infection: Infection of the transparent front layer of the eye
- Continuation of an Infection
- A corneal infection can be very dangerous to your eyesight.
- The lesions may even join forces in extreme conditions. A significant amount of skin could be lost as a result of this
A little Pox Infection Develops;
Smallpox infections can be classified as ordinary, modified, variola sine eruption, flat, or hemorrhagic by the World Health Organisation (WHO). The prevalent subtype of smallpox infections has a mortality rate of 30%.
Even in those vaccinated, mild cases of the variola sine eruption and modified subtypes are common. Although hemorrhagic and flat smallpox are very rare, they have a high mortality rate of 97%. A smallpox infection may lead to arthritis, bronchopneumonia, or viral keratitis.
MPXV
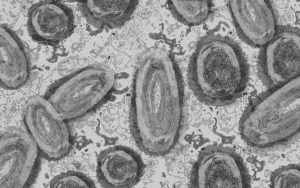
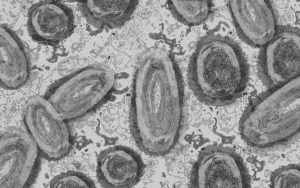
In 1958, MPXV was first discovered in lesions from cynomolgus monkeys in Denmark. In Africa in 1970, the first MPXV infection in humans was identified.
The Democratic Republic of the Congo and a few other African countries, mainly West Africa, are home to the majority of MPXV infections that have been reported.
It is significant to remember that, in addition to the 2022 outbreak discovered in more than a hundred locations worldwide, several MPXV outbreaks have been documented in the United States, the United Kingdom, and Israel between 2003 and 2018.
Analyses of the Monkeypox Virus’s DNA from Clinical Samples of Afflicted Individuals
Nigeria’s state-of-the-art laboratory is being created to combat emerging and resurgent diseases.
Investigation of the virus that causes human monkeypox
The most frequent ways for MPX to be transmitted to people are through direct contact with infected animals, contact with bodily fluids, or handling contaminated objects.
It is also known that consuming meat from an infected animal that is uncooked or undercooked might transmit the MPXV virus.
Clade II is Not the Only MPXV Clade, As Was Previously Stated;
Clade I is also a product of the Congo Basin (C.B.). Compared to other MPXV clades, CB MPXV has a higher mortality rate (11%), more frequently manifests in youngsters, and produces more severe illness.
Another recently discovered MPXV clade is Clade III, a subset of Clade II.
The symptoms of monkeypox disease resemble those of smallpox. The prodromal phase’s symptoms are submandibular, inguinal, cervical, and axillary lymphadenopathy, fever, chills, headache, sweating, myalgia, sore throat, and prostration. Lymphadenopathy is the defining feature of this illness.
MPXV-Related Skin Lesions
MPXV-induced skin lesions can spread almost as quickly as those caused by smallpox. MPXV disease is also associated with gastrointestinal symptoms. Although MPXV infection is linked to a wide variety of symptoms, about 30% of those infected exhibit no symptoms.
Dehydration from an MPXV infection can increase the risk of complications such as myocarditis, proctitis, and epiglottitis. Potential side effects of an MPXV infection include ocular damage, septic shock, and neurological impairment.
HIV Positivity is Also Found in Certain MPXV Patients.
Some people with MPXV are also HIV positive and require antiretroviral treatment. The fact that MPXV disease often occurs in association with other STDs only adds salt to injury.
Most MPXV infections during the last outbreak were mild, causing minor cutaneous lesions at the infected location. These lesions, which may be the initial sign of an infection, may emerge at various periods in different people.
Treatment
The virus that causes monkeypox has no known cure. However, smallpox therapies are sometimes employed due to the similarities between the two viruses.
Dr. Fairchok argues that most persons who contract monkeypox don’t need therapy. “But in some cases, providers may prescribe antiviral medication for groups at high risk for severe illness,” the article continues. “These groups include young children, people with weakened immune systems, pregnant women, and nursing mothers.
Although MultiCare offers treatment, they prioritise people in the above high-risk categories.
- Patients exposed to a known case of monkeypox can receive a vaccine to prevent or lessen the severity of the disease;
- however, like monkeypox treatment, vaccine supplies are limited and managed by the Washington State Department of Health.
- Dr Fairchok explains that monkeypox vaccinations have only recently arrived in Washington state and that vaccination of close contacts of any type with confirmed and suspected cases is a top priority. When vaccine supplies rise, it may expand to other high-risk populations.
- Despite promising results, clinical trials of antiviral medications for MPXV infection have been done as of yet. The anti-smallpox drug tecovirimat (ST-246), licensed by the U.S. (FDA), shows promise as a potential treatment for MPXV infection.
- The standard recommended dose of ST-246 is 600 mg, taken twice daily for 14 days. The medications can be administered through injection or taken orally. The medication interferes with the protein (p37) the conventional virus needs to encapsulate.
- The drug brincidofovir, approved by the FDA to treat smallpox illness caused by the variola virus, works by inhibiting the conventional virus’ nucleotide analogue DNA polymerase.
- The effectiveness of this drug in treating MPXV is still up for question, although it has been shown to boost survival rates when used against smallpox.
Symptomatic and supportive treatment should always be the first defence against MPXV infection.
Painful lesions, for instance, may respond well to nerve blocks, oral medications, or topical analgesics. Neurological effects of MPXV include transverse myelitis and acute disseminated encephalomyelitis (ADEM), both of which require high doses of corticosteroids to treat.
To further treat Guillain-Barré syndrome, plasmapheresis or intravenous immunoglobulin (Ig) should be administered.
Proof of Concept for a Second-Generation Smallpox Vaccine;
The efficacy of the original smallpox vaccine against MPXV is approximately 85%. There are many advantages to receiving a live vaccinia virus injection.
Still, there is also a risk of severe neurological damage. Furthermore, pregnant women, people with eczema, and people with impaired immune systems are not good candidates for live smallpox immunization.
Although two more vaccines—ACAM2000 and Jynneos—have been developed, this one is still the only one of its kind. Anyone who might come into contact with an orthopox virus should get vaccinated against it.
How lethal does the monkeypox virus tend to be?
Who is Most At Risk Because of This Threat?
McCollum claims further Research is needed to identify high-risk groups for severe monkeypox and establish transmission pathways.
Scientists investigating the 2003 Ebola epidemic in the United States, caused by the introduction of infected rodents from Ghana to pet prairie dogs in Illinois and the subsequent infection of more than seventy people, found that the severity of the disease varied depending on the route of exposure.
- It has been discovered that getting scratched or bitten by an infected animal causes more severe symptoms than inhaling respiratory droplets and particles from the animal.
- The intensity of an illness is affected by its origin;
- McCollum claims that most of the current outbreak’s illnesses have not been transferred via sexual contact.
- Whether the virus enters the body via the skin or the mucosal tissue may determine the severity of the illness.
- Zucker thinks more study is needed to see if the psychological effects of a severe case of monkeypox last long after the virus has been eradicated.
Scarring commonly forms at the sites of prior lesions, as discovered by Rogers and coworkers. According to Zucker, scarring can cause shame and depression since it can contribute to inflammation by constricting passages in the body, such as the esophagus and colon.
How to Care for a Pregnant Woman with Monkeypox
Clinical studies published by Dashraath et al. in the American Journal of Obstetrics & Gynaecology suggested that pregnant women may be at increased risk of developing monkeypox.
The extensive spread of smallpox and other orthopoxviruses posed a threat due to the possibility of vertical transmission and the lowered immunity of women of reproductive age.
In addition, the authors addressed all the conceivable complications that could arise during pregnancy. They talked about how to lessen the risk of vertical transmission by taking the monkeypox vaccine while pregnant.
In a recent letter to the editor, Mungmunpuntipantip and Wiwanitki argued against several of Dashraath et al.’s claims. They proposed alternative strategies for treating monkeypox in pregnant women, such as a focus on traditional techniques of disease prevention.
To Respond
Many of Mungmunpuntipantip and Wiwanitki’s issues were addressed in this letter. While the authors acknowledge that systemic, vaginal, or oral rashes remain the most commonly reported symptom by the World Health Organisation (WHO), they counter the assumption that clinicians are more likely to misdiagnose patients with fever and skin lesions because of unusual symptoms.
It would be premature to recommend universal screening for pregnant women without Understanding the Incidence of Asymptomatic Monkeypox Cases.
The authors responded to a question about excluding gastrointestinal symptoms from WHO surveillance reports by arguing that Mungmunpuntipantip and Wiwanitki were incorrect in characterizing the symptoms of neurological and digestive disorders as mutually exclusive.
In addition, researchers found that particularly in pregnant women, broad or frontal headache is the most common neurological sign of monkeypox.
Obstetricians were warned, however, to keep an eye out for symptoms of monkeypox virus infection, particularly those related to monkeypox-associated encephalomyelitides, such as weakness, incontinence, and mental confusion. The monkeypox virus is thought to replicate in the brains of normally healthy humans, leading to these symptoms.
NIAID


Despite the name, rodents are a common host for the monkeypox virus. The host range is unknown. However, it is associated with small African mammals like rope squirrels and huge pouched rats. In 1958, a research facility in Denmark that housed monkeys infected by rats experienced an outbreak of monkeypox.
It Resembles Smallpox in Many Ways.
- Monkeypox infections in humans were misdiagnosed as smallpox until 1970 because the symptoms were similar.
- By the decade’s conclusion, smallpox had become extremely rare thanks to eradication efforts, and increased surveillance had uncovered an uptick in instances of monkeypox.
- It was hypothesized that four of these cases resulted from direct human-to-human transmission, demonstrating the potential of such transmission.
There is a Risk of Cross-Contamination,
Mungmunpuntipantip and Wiwanitki, who both emphasized the need to correctly collect specimens, noted that not all tests for the monkeypox virus are accurate.
They stressed the importance of paying close attention to strange symptoms in light of these worries. The authors of the recent letter emphasized the importance of assessing and accrediting monkeypox testing facilities to ensure accurate results and prevent sample contamination.
Wiwanitki and Mungmunpuntipantip both mentioned smallpox illnesses and how little evidence there is of vertical transmission from mother to fetus. The monkeypox virus, it was also claimed, is too large to cross the placenta.
In Retaliation,
This study aimed to determine if monkeypox virus deoxyribonucleic acid (DNA) could be detected in fetal and placental lesions using real-time polymerase chain reaction (rt-PCR) at the time of delivery.
In addition, they suggested that socioeconomic constraints to scientific publishing in countries where the disease was once prevalent could be to blame for the absence of information on vertical transmission.
Prevention
The average recovery time for mpox is two to four weeks. Actions to alleviate symptoms and limit the spread of infections.
Do
- Remain at home, in your own room.
- Soap and water or alcohol-based hand sanitiser should be used often, especially before and after touching open wounds.
- Avoid public spaces until your rash clears up, and always wear protective gear.
- The skin should be kept dry and exposed (unless in a closed room with another person).
- Keep everything private, and regularly sanitise common areas.
- When you have mouth ulcers, you should rinse with saltwater.
- If you have a body ulcer, try a sitz or warm bath with baking soda or Epsom salts.
- Pain relievers such as ibuprofen and paracetamol (acetaminophen) are readily available over-the-counter.
Do not
- Do not scratch or pop blisters; this might delay healing and spread the rash to other body areas.
- Shave affected areas only when completely healed (otherwise, you risk spreading the rash).
- Isolating at home or in the hospital, if necessary, is the best way to prevent pox spread during the infectious phase (from the onset of symptoms until the lesions have healed and the scabs fall off).
- Lesions should be covered,
- And a medical mask should be worn publicly. Although condom use during sexual activity can lessen the likelihood of contracting pox, it cannot stop the virus from spreading through kissing or other direct skin contact.
How can we put a stop to it?
Our inability to fully understand this virus, closely related to smallpox, directly results from a lack of political will.
The 2020s have been a particularly challenging decade for studying infectious diseases. In year three of the Covid-19 pandemic, a new viral virus called monkeypox has emerged and spread widely.
Can somebody tell me if monkeypox is preventable through any kind of vaccine?
We do, however, indirectly. An immunization to one conventional virus will provide some protection against others.
- The current smallpox immunization is also effective against monkeypox because of the similarities between the two diseases.
- (Edward Jenner used less severe cowpox illnesses to create the first vaccine, which protected against the more lethal smallpox virus. Vacca, from the Latin for “cow,” is where we obtain the word “vaccine.”
- Vaccination against smallpox is available, although it is not always simple.
- The most popular vaccine against smallpox is ACAM2000, which contains a live, reproducing virus. It’s harmless for the most part, but people with compromised immune systems or skin conditions like eczema should stay away.
- Most countries discontinued vaccination programs once the number of smallpox cases began to drop because of concerns regarding adverse reactions to the vaccine.
- The good news is that a second vaccine has been created. Jynneos
- Since this vaccine contains a weakened, nonreplicating version of the virus, it may be suitable for those unable to receive the ACAM2000 vaccination.
- The only way to get full immunity from this vaccine is to have it administered twice, four weeks apart.
- Using only a fifth of the typical dose to stretch the supply has only lately begun, but the FDA has approved it.
- A further vulnerability shared by both vaccines is that neither has been tested extensively against monkeypox. Both are kept in a secure facility for use in the event of a bioterrorist attack, such as the intentional release of the smallpox virus.
- The virus’s natural ecology is little known because a study has yet to receive constant funding. Which species of animals, for instance, are most likely to disseminate the infection? I’d like to know if the reaction varies with the seasons.
We could not supply the affected countries with prophylactic immunizations because of this.
This may have protected locals from monkeypox and stopped it from spreading to countries where it doesn’t naturally occur.
Managing such an effort likely was challenging. Challenges include meeting rising demand, ensuring immunizations are lawful in all countries, and overcoming other logistical issues. However, humanity has overcome similar obstacles in the past.
- Compared to other vaccine-preventable diseases, the risk of monkeypox was quite low.
- Is there a way to prevent the spread of the disease,
- Is there a possibility that the virus might become endemic in regions other than Africa?
Public health professionals in the United States and elsewhere view this as an urgent matter of paramount importance. Vaccination and other forms of prevention have undoubtedly contributed to a gradual decline in the rate of new cases across much of the developed world, including the United States.
Where May People Get Monkeypox?
Historically, the pox virus predominated in rural, tropical areas of central and western Africa. Since 1970
Specifically, the following nations have experienced this:
- Benin
- Cameroon
- The Republic of Central Africa
- the Ivory Coast
- The Congo (Dem. Rep. of)
- Gabon
- Liberia
- Nigeria
- Central African Republic
- The Republic of Sierra Leone
- Sudan, South
- Most mpox cases have often been found in rural parts of the DRC.
- However, 87 other nations have reported pox cases as of August 2022.
- With 39,434 total cases documented worldwide, including places where the virus is uncommon.
- On July 23, 2022, the WHO will also issue a report on global health.
- The pox epidemic has prompted the declaration of a public health emergency of international concern.
How Can Monkeys Get the Disease?
The following substances can facilitate the transmission of the pox virus:
- blood
- fluids of the body
- cuts, sores, and other wounds
- sputum, for interpersonal communication between humans
- The pox virus can also be transmitted through contact with infected objects, fabrics, or surfaces.
- The virus can potentially cross the placenta and infect the developing baby of a pregnant woman.
That’s what the CDC (Centres for Disease Control and Prevention) folks say, anyway.
- Intimate contact, kissing, or cuddling can also transfer the mpox virus.
- touch (as in a hug, a massage, or a kiss)
- Sexual contact of any sort
- Contact with a pox-infected person’s genitalia or anus.
- extensive periods of face-to-face interaction and sexual contact with an infected object, such as a partner, a bed, a towel, or a sex toy
Additional modes of transmission include:
- Animal pox is transmitted through bites and scratches.
- Consuming meat from an infected animal
- How monkeypox spreads through the respiratory system and whether or whether it may be transmitted by contact with other bodily fluids such as vaginal fluids, sperm, urine, or feces are all questions that are still being investigated by scientists.
- Cytomegalovirus eye infections are routinely treated with cidofovir, which has also been utilized in some mumps cases.
Some other therapies centre on
- On relieving discomfort with over-the-counter or prescribed drugs such as anti-inflammatory drugs, pain relievers, and antihistamines.
- Can monkeypox be avoided by vaccination?
The effectiveness of the smallpox vaccine is estimated by the WHO to be 85 percent.
Able to halt the spread of pox effectively. If you were vaccinated against smallpox as a child and subsequently caught pox, you might experience minimal symptoms.
Two vaccines are currently in development and could be utilized.
JYNNEOS and ACAM2000 are effective vaccines for preventing pox.
People exposed to pox or at a higher risk of being affected by the virus should get vaccinated.

These folks include those who:
- Having been identified as a close contact of a pox patient by public health authorities
- Have had a partner during the past two weeks who has tested positive for pox
- have had at least three partners in sexual activity in the last two weeks in a region with confirmed cases of pox
- Who works in environments where they may be exposed to orthopoxviruses like pox?
- The (CDC) also recommends vaccination for everyone who has had intimate contact with someone with mumps.
- To prevent mumps, you should regularly wash your hands and avoid persons who have them or anything they may have touched.
Who should be tested for monkeypox, and how can you tell if you have it?
- Suggests getting advice from a medical expert to determine if testing is required.
- Diseases are identified by doctors.
- Pox using a combination of techniques:
- Examining fluid from lesions or crusted scabs in a laboratory. A polymerase chain reaction (PCR) test can detect the virus in these specimens.
- To conduct a biopsy, a small skin sample is surgically removed and then tested for the presence of the virus.
- In most cases, a blood test is unnecessary. This is due to the short half-life of the pox virus in the blood. As a result, there are more reliable methods for detecting mpox.
Frequently Asked Questions,
Can you explain what monkeypox is?
Monkeypox is a viral infection from the same family as the smallpox virus. “It is self-limiting, so the infection should clear itself as time passes.”
How does it go around?
Most cases of monkeypox today are found in guys who engage in homosexual acts with other men. Dr Michael Chang, a paediatric infectious disease specialist at Houston’s Memorial Hermann, insists that no one is completely safe from contracting monkeypox. It does not discriminate based on age, health, or sexual orientation.
- Whether young or old, healthy or immunocompromised, “monkeypox can spread to anyone.” adds Chang.
- Skin-to-skin contact is the major means of transmission, according to Chang. This communication may consist of:
- The primary risk factor for contracting monkeypox is coming into touch with an infected person showing symptoms of the disease.
- Intimate physical touch such as sexual encounters, embraces, kisses, or lengthy face-to-face interaction
- Contact with unclean surfaces, items of clothing, and linens used by a person infected with monkeypox; this transmission route is less common than the others.
- According to Chang, the virus can even cross the placenta and infect the unborn child.
The current outbreak differs from previous ones because “Contact with infected animals was the leading cause of monkeypox in children.” says Chang. The source of a 2003 outbreak in the United States was determined to be infected prairie dogs.
Is monkeypox contagious?
The monkeypox virus does not spread through sexual contact. Erica Susky, a Toronto-based infection control specialist, counters that the term should be used more.
The common belief is that HPV only spreads through sexual contact. However, Susky argues that close, non-sexual relationships can also serve as vectors. Examples include hugging, kissing, and making close eye contact with someone.
Nonetheless, these interactions might not be sexual, but they nonetheless present a chance for the spread of disease.
Though monkeypox can be transmitted sexually, skin-to-skin contact is the major transmission mechanism. Hence, it is not classified as a sexually transmitted infection.
Can monkeypox cause death?
The monkeypox that Dr. Douglas Chiriboga treats at Pomona Valley Hospital Medical Centre is “rarely fatal,” he says. “At this time, we are dealing with West African monkeypox.”
However, Chiriboga and others stress that some groups are especially vulnerable to death.
“For unvaccinated kids and others with impaired immune systems, it can be fatal,” warns Chang.
Cox also notes that between 1 and 10% of the population has been lost in prior epidemics.
Cox said scientists are learning more about managing the sickness and preventing serious complications.
Can you get over monkeypox?
Dr Jay Varma, the director of the Cornell Centre for Pandemic Prevention and Response and a Kroll Institute Fellow, emphasises that monkeypox currently has no recognised cure.
But there are remedies available. Varma said doctors can get Tecovirimat (TPOXX) from the Centres for Disease Control and Prevention.
Some patients who were given this medication during the epidemic said it accelerated the healing of their rash and significantly reduced their pain.
Cox reaffirmed that monkeypox has a natural lifespan of a few weeks.
After two to four weeks, “monkeypox generally goes away on its own,” adds Cox. To be more specific: “However, children and those with some medical conditions may become more seriously ill.”
Is there protection against monkeypox?
Varma claims that the two currently used smallpox vaccinations, which have been demonstrated to be effective against monkeypox, are being administered to the general public.
The anti-varicella vaccination ACAM2000
The more recent vaccination, JYNNEOS
Although data is scarce, the vaccine is thought to be about 85% effective in preventing monkeypox.
To better evaluate how protective the vaccine is, “researchers are doing studies on patients during this outbreak,” Varma explains.
Those who are recommended to get vaccinated by the CDC are:
Have recent contact with monkeypox (4-14 days ago)
Hold particular occupations, such as those in laboratories where animals with orthopoxviruses are handled directly, putting humans at risk of infection.
Why does monkeypox pose such a threat to public health right now?
Why are states declaring emergencies if monkeypox has such a low mortality rate?
The World Health Organisation (WHO) has issued a rare global health emergency declaration; why?
- “”In most individuals, monkeypox causes severe agony and anguish for weeks,” Varma explains.
- Sometimes, the pain is so terrible that you need to be hospitalised;
- sometimes, the rash leaves scars on your skin or gets infected with bacteria;
- sometimes, the sickness damages your brain, eyes, and lungs.
Varma adds that in the case of other viruses, including COVID-19, other impacts, such as long COVID-19, were not discovered until much later by healthcare providers and scientists.
Susky emphasises that the risk is especially high for the young and the immunocompromised.
What is the incubation period for monkeypox?
According to Varma, monkeypox carriers remain infectious until the rash entirely fades.
According to him, this indicates that the blister has healed, the scab has peeled off, and new skin has grown.